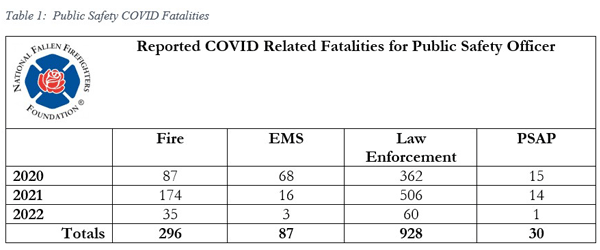
 Although the global pandemic has officially been declared over, many organizations continue to struggle with the lingering impact of COVID-19 infection and pandemic-related disruptions on the workforce. During the pandemic, fire service agencies, especially those doing EMS work, were plagued with employee exposures, illnesses, and the need to quarantine responders. In some cases, these illnesses lead to fatalities. Table 1 provides a listing of reported emergency service COVID fatalities through 2022 as tabulated by the National Fallen Firefighters Foundation.
Although the global pandemic has officially been declared over, many organizations continue to struggle with the lingering impact of COVID-19 infection and pandemic-related disruptions on the workforce. During the pandemic, fire service agencies, especially those doing EMS work, were plagued with employee exposures, illnesses, and the need to quarantine responders. In some cases, these illnesses lead to fatalities. Table 1 provides a listing of reported emergency service COVID fatalities through 2022 as tabulated by the National Fallen Firefighters Foundation.
Throughout the pandemic, a major struggle for departments was determining whether infection and illness due to COVID-19 occurred from duty-related exposure or whether the firefighter became ill from an off-duty interaction. This lack of clarity produced challenging questions as to how to charge leave time (sick leave or workers compensation) and, in some cases, led to questions about whether the death of a firefighter was duty-related, or part of a disease process not directly linked to their work as a firefighter and EMS provider. Workers’ compensation providers weighed in, providing advice to governmental leaders that often seemed focused on limiting claim exposure. Fortunately, we have learned much from those early days of the pandemic, but challenges remain.
Long COVID, as it is commonly known, is a condition of prolonged symptoms experienced by those who have moved beyond the generalized illness phase and are now plagued with chronic, and sometimes debilitating, ongoing medical conditions. These patients, often called “long haulers” require continued medical care, off-duty leave time, and in some cases short- and long-term disability. One of the great mysteries about Long COVID is the myriad symptoms that can be related to it. Although there have been over 50 symptoms/conditions linked to Long COVID, the most common include extreme fatigue, lingering respiratory conditions, neurocognitive impairments (brain fog), and multiple cardiac conditions. Of course, many of these problems can be caused by health conditions other than COVID-19, further complicating the diagnosis and treatment. Figure 1 highlights the ways in which Long COVID can impact the body systems, leading to an array of symptoms, which can collectively impair firefighter health and safety.
Of great concern to fire chiefs are the firefighters who, based on their symptoms, should not be actively engaged in emergency service delivery. Unfortunately, anecdotal evidence suggests that many return to work and struggle through the challenges because no mechanism exists to provide for their continued use of leave time or assignment to a light duty position. There is concern that these members may be able to manage station duties without much trouble, but, if maximally stressed at the scene of a complex incident, could become a safety risk to both themselves as well as their fellow firefighters.
Further obscuring a full view of the health challenges associated with COVID-19 is the emerging evidence that COVID-19 illness increases the risk of cardiac conditions; this is true among those with symptoms and without “classic” Long COVID symptoms. The cardiopulmonary health of firefighters has been a concern for many years. But there is a heightened reason for concern now as research has found that infection with COVID-19 can lead to a 40%-60% increased risk of cardiovascular events a year or more after initial infection (Wan et al., 2023; Xie et al., 2022). These complications include a risk for several types of dysrhythmias with a close to two-fold increased risk in this general category (Xie et al., 2022). Clotting has also emerged as a significant concern post-COVID, supported by data that shows risk of pulmonary embolism and deep vein thrombosis is over 2-3 times greater in those who had COVID-19 compared to those who did not (Xie et al., 2022).
Not only is the struggle real for those dealing with the debilitating symptoms of Long COVID, but the fact is that fire service leaders have few good options to assist their affected personnel while still maintaining essential services. Many departments report that their new firefighter recruitment is at an all-time low. Many paid departments are operating with multiple vacancies and are unable to find new recruits. Likewise, volunteer departments are struggling to find community members interested in joining their ranks and serving their communities. This reality does not afford fire service leaders as much leeway in attending to the needs of firefighters who may need extra time for recovery.
In many ways the pandemic brought to light the risks to essential employees (both paid or volunteer firefighters) causing new candidates to rethink their willingness to expose themselves and their families to the health concerns of diseases such as COVID -19. This lack of staffing is resulting in a workforce that is exhausted due to rampant overtime or, in the case of the volunteer service, only a handful of members doing most of the work. Two recent examples shared with the authors highlight the impact of short staffing.
- A busy fire protection district located in a southern state reported in 2022 that their personnel, although assigned a 24/48 shift schedule, generally worked a 48/24 schedule to keep their fire and ambulance companies operational. This only gave the personnel a brief 24-hour “off-duty” period to recuperate before returning and doing it again. Often, they did not even get the 24-hours off which resulted in some members working 120 hours straight.This continued workload has caused both attrition and employee turnover, which has exacerbated the problem since the new candidate pool is already extremely low.
- A Midwest department noted a massive increase in mandatory overtime (firefighters ordered to work overtime). This department saw 5.6 times increase in mandatory overtime between 2019 and 2022. This was driven by COVID-related illnesses and attrition which resulted in the department being extremely short-staffed. Further exacerbating the situation was the fact that the City leadership decided to not fill vacancies occurring during the pandemic due to concerns over their long-term financial stability.
Bottom line, without adequate staffing, fire service leaders are unable to accommodate the leave time/recuperation time needed by those experiencing the symptoms of Long COVID. With symptomatic firefighters needing additional leave time or modified schedules and the fact that we are generally unable to find candidates interested in filling vacancies, the fire service finds itself in a very challenging situation.
There is well-researched evidence that shows that increases in mandatory firefighter overtime ultimately leads to increased sick leave usage. The late Don Abbott in his Project Mayday Study documents that 53.6% of all firefighter maydays were called by firefighters working overtime. Worker’s compensation insurance providers have data showing a linkage between overtime and increases in firefighter injuries including a connection between vehicle crashes and the number of hours of wakefulness by emergency service workers. Consistently, the second leading cause of firefighter fatalities is motor vehicle accidents – accounting for 20% to 25% of all line-of-duty deaths every year. Now add the health challenges of those suffering persistent Long COVID symptoms, including cardiorespiratory compromise and “brain fog” to the known risks of excessive overtime, and the resulting situation is unsustainable.
When applying a risk management overlay to our current situation, the fire and emergency service profession, regardless of whether it is paid or volunteer, finds itself in a very precarious position. Certainly, additional research is needed to fully understand the lasting impact of COVID-19 illness on firefighter health and to truly understand the full impact of the pandemic on the emergency services. Fire service leaders must also seek to understand the situation, mitigate it to the best of their ability, and look for additional resources to truly address the needs they face.
A 360-degree assessment is standard protocol during the first minutes on the fireground; it provides awareness of the problem. Similarly, the first step in addressing Long COVID needs to be awareness. The complex and nonspecific nature of Long COVID may even mean that firefighters who are dealing with new health issues post-COVID are not connecting these problems with a potential diagnosis of Long COVID. That is the first step towards treatments that are emerging. Unfortunately, there is currently no cure, but Long COVID treatment centers have emerged across the U.S. and researchers, including those within the fire service, are aggressively pursuing answers. Recognition that Long COVID impacts coworkers and employees can help the department connect members with information on care, recovery, research, rehabilitation, support groups, and disability benefits (two of the many websites with this type of information are listed below). The pandemic may have been officially declared over, but the impact on the fire service remains a challenge for many. For fire service leaders, options for addressing these challenges may be limited and difficult, but overlooking the problem will not move the department towards a solution.
Resources:
cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
longhauler-advocacy.org
References:
Wan, E. Y. F., Mathur, S., Zhang, R., Yan, V. K. C., Lai, F. T. T., Chui, C. S. L., Li, X., Wong, C. K. H., Chan, E. W. Y., Yiu, K. H., & Wong, I. C. K. (2023). Association of COVID-19 with short- and long-term risk of cardiovascular disease and mortality: A prospective cohort in UK biobank. Cardiovascular Research, cvac195.
Xie, Y., Xu, E., Bowe, B., & Al-Aly, Z. (2022). Long-term cardiovascular outcomes of COVID-19. Nature Medicine, 28(3)
Authors: Chief Craig A. Haigh (Ret.), Sue D’Isabel, DrPH and Denise Smith, PhD
Craig A. Haigh is a retired fire chief from the Chicago Metro Area and now works full-time as a consultant focused on organizational management. He has been involved in firefighter health and safety research for more than 20 years focusing specifically on procedures to implement research findings into emergency service operations. He is the Author of the book The Dynamic Fire Chief: Principles for Organizational Management and has published over 50 fire service trade journal articles.
Sue D’Isabel is a project manager for a FEMA-AFG project focused on firefighter health and safety through the First Responder Health and Safety Laboratory at Skidmore College in Saratoga Springs, New York. She has taught public health courses in Skidmore’s Health and Human Physiological Sciences Department for over 10 years.
Denise Smith is a professor of health and human physiological sciences and director
of the First Responder Health and Safety Laboratory at Skidmore College in Saratoga
Springs, New York; a senior research scientist at the University of Illinois Fire Service
Institute; and has conducted more than 40 firefighter fatality investigations for the NIOSH Fire Fighter Fatality Investigation and Prevention program. Smith has coauthored two major textbooks, published more than 100 scientific articles, and been awarded more than $14 million in research funding.
Download article (PDF)